Елена Беликова
Английский язык для медиков
1. History of medicine
Medicine is among the most ancient of human occupations. It began as an art and gradually developed into a science over the centuries. There are 3 main stages in medicine development: Medicine of Ancient Civilizations, Medicine of Middle Ages and Modern Medicine.
Early man, like the animals, was subject to illness and death. At that time medical actions were mostly a part of ceremonial rituals. The medicine—man practiced magic to help people who were ill or had a wound. New civilizations, which developed from early tribes, began to study the human body, its anatomic composition. Magic still played an important part in treating but new practical methods were also developing. The early Indians, e. g., set fractures and practiced aromatherapy. The Chinese were pioneers of immunization and acupuncture. The contribution of the Greeks in medicine was enormous. An early leader in Greek medicine was Aesculapius. His daughters, Hygeia and Panacea gave rise to dynasties of healers (curative medicine) and hygienists (preventive medicine). The division in curative and preventive medicine is true today. The ethic principles of a physician were summarized by another Greek, Hippocrates. They are known as Hippocrates Oath.
The next stage of Medicine's development was the Middle Ages. A very important achievement of that time was the hospital. The first ones appeared in the 15–th century in Oriental countries and later in Europe. Another advance of the Middle Ages was the foundation of universities during 13–14–th centuries. Among other disciplines students could study medicine. During 18–th century new discoveries were made in chemistry, anatomy, biology, others sciences. The advances of that time were invention of the stethoscope (by Rene Laennec), vaccination for smallpox, discovery of anesthetics and development of immunology and scientific surgery. The next century is rise of bacteriology. Important discoveries were made by Louis Pasteur and Robert Koch. The development of scientific bacteriology made possible advances in surgery: using antiseptics and control of wound infection.
Medicine in the 20–th century made enormous contribution in the basic medical sciences. These are discovery of blood groups and vitamins, invention of insulin and penicillin, practice of plastic surgery and transplantation.
New words
medicine – медицина
human – человеческий
occupation – занятие
to develop – развивать
science – наука
civilization – цивилизация
Middle аges – Средние века
modern – современный
animal – животное
illness – заболевание
death – смерть
discovery – открытие
blood – кровь
Early man, like the animals, was subject to illness and death. At that time medical actions were mostly a part of ceremonial rituals. The medicine—man practiced magic to help people who were ill or had a wound. New civilizations, which developed from early tribes, began to study the human body, its anatomic composition. Magic still played an important part in treating but new practical methods were also developing. The early Indians, e. g., set fractures and practiced aromatherapy. The Chinese were pioneers of immunization and acupuncture. The contribution of the Greeks in medicine was enormous. An early leader in Greek medicine was Aesculapius. His daughters, Hygeia and Panacea gave rise to dynasties of healers (curative medicine) and hygienists (preventive medicine). The division in curative and preventive medicine is true today. The ethic principles of a physician were summarized by another Greek, Hippocrates. They are known as Hippocrates Oath.
The next stage of Medicine's development was the Middle Ages. A very important achievement of that time was the hospital. The first ones appeared in the 15–th century in Oriental countries and later in Europe. Another advance of the Middle Ages was the foundation of universities during 13–14–th centuries. Among other disciplines students could study medicine. During 18–th century new discoveries were made in chemistry, anatomy, biology, others sciences. The advances of that time were invention of the stethoscope (by Rene Laennec), vaccination for smallpox, discovery of anesthetics and development of immunology and scientific surgery. The next century is rise of bacteriology. Important discoveries were made by Louis Pasteur and Robert Koch. The development of scientific bacteriology made possible advances in surgery: using antiseptics and control of wound infection.
Medicine in the 20–th century made enormous contribution in the basic medical sciences. These are discovery of blood groups and vitamins, invention of insulin and penicillin, practice of plastic surgery and transplantation.
New words
medicine – медицина
human – человеческий
occupation – занятие
to develop – развивать
science – наука
civilization – цивилизация
Middle аges – Средние века
modern – современный
animal – животное
illness – заболевание
death – смерть
discovery – открытие
blood – кровь
2. Cell
The cell is a smallest independent unit in the body containing all the essential properties of life. Man у types of human cells can be grown in test tubes after beeing taken from the body. Cells which are functionally organized are often grouped together and operate in concert as a tissue, such as muscle tissue or nervous tissue. Various tissues may be arranged together to form a unit called organ as the kidney, liver, heart or lungs. Organs often function in groups called organ systems. Thus the esophagus, stomach, раn—сreаs, liver and intestines constitute the digestive system.
Cells are characterized by high degree of complexity and order in both structure and function. The cell contains a number.
Of structures called cell organelles. These are responsible for carrying out the specialized biochemical reactions characterizing each. The many chemical reactions taking place in a cell require the establishment of varied chemical microenvironment.
Carefully controlled transport mechanisms along with highly effective barriers – the cell membranes – ensure that chemicals are present in the proper region of the cell in appropriate concentration.
The cell membranes of a mixture of protein and lipid form its surroundings.
Membranes are an essential component of almost all cells organelles. The membrane allows only certain molecules to pass through it.
The most visible and essential organelle in a cell is the nucleus, containing genetic material and regulating the activities of the entire cell.
The area outside of the molecules is called the cytoplasm. Cytoplasm contains a variety of organelles that have different functions.
New words
cell – клетка
independent – независимый
unit – единица
body – тело
all – все
lipid – жир
microenvironment – микровооружение
muscle – мышечный
nervous – нервный
digestive – пищеварительный
life – жизнь
human – человеческий
together – вместе
tissue – ткань
organ systems – системы органов
to function – функционировать
to contain – содержать
membranes – мембраны
protein – протеин
nucleus – ядро
cytoplasm – цитоплазм
different – различный
Cells are characterized by high degree of complexity and order in both structure and function. The cell contains a number.
Of structures called cell organelles. These are responsible for carrying out the specialized biochemical reactions characterizing each. The many chemical reactions taking place in a cell require the establishment of varied chemical microenvironment.
Carefully controlled transport mechanisms along with highly effective barriers – the cell membranes – ensure that chemicals are present in the proper region of the cell in appropriate concentration.
The cell membranes of a mixture of protein and lipid form its surroundings.
Membranes are an essential component of almost all cells organelles. The membrane allows only certain molecules to pass through it.
The most visible and essential organelle in a cell is the nucleus, containing genetic material and regulating the activities of the entire cell.
The area outside of the molecules is called the cytoplasm. Cytoplasm contains a variety of organelles that have different functions.
New words
cell – клетка
independent – независимый
unit – единица
body – тело
all – все
lipid – жир
microenvironment – микровооружение
muscle – мышечный
nervous – нервный
digestive – пищеварительный
life – жизнь
human – человеческий
together – вместе
tissue – ткань
organ systems – системы органов
to function – функционировать
to contain – содержать
membranes – мембраны
protein – протеин
nucleus – ядро
cytoplasm – цитоплазм
different – различный
3. Tissue
A tissue is a group of cells working together to do a special job. A histologist is one who specializes in the study of tissues. The cells, of which the tissues are made, contain from 60 to 99 % water. Chemical reactions that are necessary for proper body function are carried on much more readily in a water solution. The water solution and other materials in which the tissues are bathed is slightly salty. It must be mentioned that an insufficiency of tissues fluid is called dehydration and an abnormal accumulation of this fluid caused a condition called edema.
Tissue classification: The 4 main groups of tissues are:
1) epithelial tissue forms elands, covers surfaces and lines cavities;
2) connective tissue holds all parts of the body in Place. This can be fat, cartilage, bone or blood. Blood sometimes is considered a sort of tissue, since it contains cells and performs many of the functions of tissues. However; the blood has many other unique characteristics;
3) nerve tissue conducts nerve impulses all over the body;
4) the muscle tissue is designed for power—producing contractions.
The surface of the body and of the tubes or passages leading to the exterior and the surface of the various cavities in the body are lined by cells which are closely approximated to each other; thus have a small amount of intercellular substance. This lining cellular layer is called epithelium. The nature and consistency of intercellular substance, the matrix, and the amount and arrangement of fibers furnish the basis for the subdivision of connective tissue into three main groups: connective tissue proper, cartilage and bone. In connective tissue the intercellular substance is soft; in cartilage it is firm, yet flexible and ela stic; in bone it is rigid due to the deposition of calcium salt in the matrix. In multicellular organisms certain cells developed to a high degree the properties of irritability and conductivity. These cells form the nervous tissues.
The nervous system of higher animals is characterized by the multiplicity of cellular forms and intercellular connections and by the complexity of its functioning.
Muscle tissue is composed of elongated cells which have the power of contracting or reducing their length. This property of contraction is ultimately a molecular phenomenon and is due to the presence of protein molecules. The following three types of muscle tissue occur in the body.
Smooth muscle tissue is found in sheet or tubes forming the walls of many hollow or tubular organs, for example the bladder, the intes tines of blood vessels. The cells forming this tissue are long spin dles with a central oval nucleus.
Striated muscle tissue is composed of cylindrical fibres often of great at length in which separate cells cannot be distinguished. Many small nuclei are found in the fibres lie just under the surface. Cardiac muscle resembles striated muscle in its structure, but smooth one in its action.
New words
liquid – жидкость
epithelial – эпителиальный
layer – слой
muscle – мышца
body – тело
flexible – гибкий
elastic – эластичный
nucleus – ядро
smooth – гладкий
fibre – волокно
cardiac – сердечный
Tissue classification: The 4 main groups of tissues are:
1) epithelial tissue forms elands, covers surfaces and lines cavities;
2) connective tissue holds all parts of the body in Place. This can be fat, cartilage, bone or blood. Blood sometimes is considered a sort of tissue, since it contains cells and performs many of the functions of tissues. However; the blood has many other unique characteristics;
3) nerve tissue conducts nerve impulses all over the body;
4) the muscle tissue is designed for power—producing contractions.
The surface of the body and of the tubes or passages leading to the exterior and the surface of the various cavities in the body are lined by cells which are closely approximated to each other; thus have a small amount of intercellular substance. This lining cellular layer is called epithelium. The nature and consistency of intercellular substance, the matrix, and the amount and arrangement of fibers furnish the basis for the subdivision of connective tissue into three main groups: connective tissue proper, cartilage and bone. In connective tissue the intercellular substance is soft; in cartilage it is firm, yet flexible and ela stic; in bone it is rigid due to the deposition of calcium salt in the matrix. In multicellular organisms certain cells developed to a high degree the properties of irritability and conductivity. These cells form the nervous tissues.
The nervous system of higher animals is characterized by the multiplicity of cellular forms and intercellular connections and by the complexity of its functioning.
Muscle tissue is composed of elongated cells which have the power of contracting or reducing their length. This property of contraction is ultimately a molecular phenomenon and is due to the presence of protein molecules. The following three types of muscle tissue occur in the body.
Smooth muscle tissue is found in sheet or tubes forming the walls of many hollow or tubular organs, for example the bladder, the intes tines of blood vessels. The cells forming this tissue are long spin dles with a central oval nucleus.
Striated muscle tissue is composed of cylindrical fibres often of great at length in which separate cells cannot be distinguished. Many small nuclei are found in the fibres lie just under the surface. Cardiac muscle resembles striated muscle in its structure, but smooth one in its action.
New words
liquid – жидкость
epithelial – эпителиальный
layer – слой
muscle – мышца
body – тело
flexible – гибкий
elastic – эластичный
nucleus – ядро
smooth – гладкий
fibre – волокно
cardiac – сердечный
4. Epidermis
The integument consists of the skin (epidermis and der—mis) and associated appendages (sweat glands, sebaceous glands, hairs, and nails). Considered the largest body organ, the integument comprises approximately 16 % of total body weight. It is a highly specialized organ that functions to protect the body from injury, desiccation, and infection. It also participates in sensory reception, excretion, thermoregulation, and maintenance of water balance.
Epidermis is the outermost layer of the integument. It is astratified squamous epithelial layer of ectodermal origin.
Layers of the epidermis from deep to superficial consist of four strata. Stratum basale (stratum germinativum) is a proliferative basal layer of columnar—like cells that contain the fibrous protein keratin. Stratum spinosum is a multilaminar layer of cuboidal—like cells that are bound together by means of numerous cytoplasmic extensions and desmosomal junctions.
Stratum granulosum consists of flat polygonal cells filled with basophilic keratohyalin granules. Viewed at the electron microscopic level, these cells also contain numerous mem brane—coating granules. Stratum corneum is the superficial stratum of dead cells and consists of several to many layers of flat, anucleated, and cornified (kera—tinized) cells. In the epidermis of the palms and soles, a thin, transitional zone of flat eosinophilic or pale—staining anucleated cells may occur as the stratum lucidum. This layer is found only in regions with a thick strata cor—neum.
Cells of the epidermis: keratinocytes are the most numerous and are responsible for the production of the family of keratin proteins that provide the barrier function of the epidermis.
Melanocytes are derivatives of neural crest ectoderm. They are found in the dermis and are also scattered among the keratinocytes in the basal layers of the epidermis. These dendritic cells produce the pigment melanin in the form melanosomes that are transferred to keratinocytes.
Langerhans cells are dendritic cells but are members of the immune system and function as antigen—presenting cells. They have also been found in other parts of the body, including the oral cavity and lymph nodes.
Merkel cells are found in the basal epidermis and appear function in concert with nerve fibers that are closely associated with them. At the electron microscopic level, their cytoplasm contains numerous membrane—bound granules that resemble those of catecholamine—produ—cing cells.
New words
epidermis – эпидермис dermis – дерма weight – вес to protect – защищать injury – рана
cytoplasmic – цитоплазматический
level – уровень
flat – плоский
palm – ладонь
thick – толстый
pigment – пигмент
melanin – меланин
nerve – нерв
Epidermis is the outermost layer of the integument. It is astratified squamous epithelial layer of ectodermal origin.
Layers of the epidermis from deep to superficial consist of four strata. Stratum basale (stratum germinativum) is a proliferative basal layer of columnar—like cells that contain the fibrous protein keratin. Stratum spinosum is a multilaminar layer of cuboidal—like cells that are bound together by means of numerous cytoplasmic extensions and desmosomal junctions.
Stratum granulosum consists of flat polygonal cells filled with basophilic keratohyalin granules. Viewed at the electron microscopic level, these cells also contain numerous mem brane—coating granules. Stratum corneum is the superficial stratum of dead cells and consists of several to many layers of flat, anucleated, and cornified (kera—tinized) cells. In the epidermis of the palms and soles, a thin, transitional zone of flat eosinophilic or pale—staining anucleated cells may occur as the stratum lucidum. This layer is found only in regions with a thick strata cor—neum.
Cells of the epidermis: keratinocytes are the most numerous and are responsible for the production of the family of keratin proteins that provide the barrier function of the epidermis.
Melanocytes are derivatives of neural crest ectoderm. They are found in the dermis and are also scattered among the keratinocytes in the basal layers of the epidermis. These dendritic cells produce the pigment melanin in the form melanosomes that are transferred to keratinocytes.
Langerhans cells are dendritic cells but are members of the immune system and function as antigen—presenting cells. They have also been found in other parts of the body, including the oral cavity and lymph nodes.
Merkel cells are found in the basal epidermis and appear function in concert with nerve fibers that are closely associated with them. At the electron microscopic level, their cytoplasm contains numerous membrane—bound granules that resemble those of catecholamine—produ—cing cells.
New words
epidermis – эпидермис dermis – дерма weight – вес to protect – защищать injury – рана
cytoplasmic – цитоплазматический
level – уровень
flat – плоский
palm – ладонь
thick – толстый
pigment – пигмент
melanin – меланин
nerve – нерв
5. Dermis
Dermis is a connective tissue layer of mesodermal origin subjacent the epidermis and its basement membrane. The dermis—epidermal junction, especially in thick skin, is characterized by numerous papillary interdigitations of the dermal connective tissue and epidermal epithelium. This increases the surface area of attachment and brings blood vessels in closer proximity to the epidermal cells. The epidemis, like epithelia in general, is devoid of blood vessel. Histologically, dermis consists of two identifiable regions.
Papillary layer, associated principally with the dermal papillae, is the most superficial layer. It consists of a loosely packed, irregular meshwork of collagen fibrils that contain fine blood vessels and nerve endings.
Reticular layer is the deeper dermal layer and consists of coarse collagen bundles intertwined with elastic fibers in a gel matrix. This layer is a typical dense irregular connective tissue.
HYPODERMIS: this layer of loose vascular connective tissue is infiltrated with adipocytes and corresponds to the superficial fascia of gross anatomy. However, since it contains the deepest portions of the cutaneous glands and hairs, it is also an important part of the skin. The hypoder—mis fastens the skin to underlying muscles and other structures.
New words
dermis – дерма connective – соединительный membrane – мембрана junction – соединение
to be characterized by – характеризоваться чем—то numerous – значительный
to increase – увеличивать
surface – поверхность area – площадь epidermal – эпидермальный thick – толстый skin – кожа
papillary – папиллярный devoid – происходить meshwork – ячеистая сеть coarse – грубый bundle – связка interwine – сплетаться bring – приносить to consists of – состоять из to contain – содержать collagen – коллагеновый adipocyte – жировая клетка
Papillary layer, associated principally with the dermal papillae, is the most superficial layer. It consists of a loosely packed, irregular meshwork of collagen fibrils that contain fine blood vessels and nerve endings.
Reticular layer is the deeper dermal layer and consists of coarse collagen bundles intertwined with elastic fibers in a gel matrix. This layer is a typical dense irregular connective tissue.
HYPODERMIS: this layer of loose vascular connective tissue is infiltrated with adipocytes and corresponds to the superficial fascia of gross anatomy. However, since it contains the deepest portions of the cutaneous glands and hairs, it is also an important part of the skin. The hypoder—mis fastens the skin to underlying muscles and other structures.
New words
dermis – дерма connective – соединительный membrane – мембрана junction – соединение
to be characterized by – характеризоваться чем—то numerous – значительный
to increase – увеличивать
surface – поверхность area – площадь epidermal – эпидермальный thick – толстый skin – кожа
papillary – папиллярный devoid – происходить meshwork – ячеистая сеть coarse – грубый bundle – связка interwine – сплетаться bring – приносить to consists of – состоять из to contain – содержать collagen – коллагеновый adipocyte – жировая клетка
6. Cutaneous appendages
Cutaneous appendages are all derivatives of the epidermis.
Eccrine (merocrine) sweat glands are simple, coiled, tubular glands that are widely distributed over the body. Secretory portions are tightly coiled and consist of a single layer of columnar—like pyramidal cells.
Duct portions, composed of two cuboidal cell layers, are corkscrew—shaped and open onto the epidermal surface. These glands are important in thermal regulation.
Control of the eccrine glands is mainly by the innerva—tion of cholinergic fibers.
Apocrine sweat glands are also simple, coiled, tubular glands but are much less abundant in their distribution than eccrine glands. They can be found in the axillary, ar—eolar, and anal regions.
Secretory portions of these glands are composed of a single layer of cuboidal or columnar cells. They are larger and have a much wider luminal diameter than eccrine sweat glands. Myoepithelial cells surround the secretory cells within the basement membrane and contract to facilitate secretion.
Duct portions are similar to those of eccrine sweat glands but open onto hair follicles instead of onto the epidermal surfaces.
Functions of these glands in humans is not at all clear. Specialized apocrine glands in the ear canal (ceruminous glands) produce a secretion in conjunction with adjacent sebaceous glands to form the protective earwax (cerumen). Control of the apocrine glands is hormonal and via the innervation of adrenergic fibers. These glands do not begin to function until puberty.
Sebaceous glands are simple, branched holocrine aci—nar glands. They usually discharge their secretions onto the hair shaft within hair follicles. These glands are found in the dermis throught the skin, except on the palms and soles.
Secretory portions consist of peripherally located, flattened stem cells that resemble basal keratinocytes. Toward the center of the acini, enlarged differentiated cells are engorged with lipid. Death and fragmentation of cells nearest the duct portion result in the holocrine mechanism of secretion.
Duct portions of sebaceous glands are composed of stratified squamous epithelium that is continuous with the hair cat and epidermal surface.
Functions involve the lubrication of both hairs and corni—fied layers of the skin, as well as resistance to desiccation.
Control of sebaceous glands is hormonal. Enlargement of the acini occurs at puberty.
Hairs are long, filamentous projections consisting of dead keratini—zed epidermal cells. Each hair derives from an epidermal invagination called the hair follicle, which possesses a terminal hair bulb, located in the dermis or hypo—dermis, from which the hair shaft grows. Contraction of smooth muscles raise the hairs and dimple the epidermis («goose flesh»).
Nails, like hair, are a modified stratum corneum of the epidermis. They contain hard keratin that forms in a manner similar to the formation of hair. Cells continually proliferate and keratinize from the stratum basale of the nail matrix.
New words
cutaneous – кожный
appendace – покров
tubular – трубчатый
pyramidal – пирамидальный
surface – поверхность
thermal – тепловой
innervation – иннервация
Eccrine (merocrine) sweat glands are simple, coiled, tubular glands that are widely distributed over the body. Secretory portions are tightly coiled and consist of a single layer of columnar—like pyramidal cells.
Duct portions, composed of two cuboidal cell layers, are corkscrew—shaped and open onto the epidermal surface. These glands are important in thermal regulation.
Control of the eccrine glands is mainly by the innerva—tion of cholinergic fibers.
Apocrine sweat glands are also simple, coiled, tubular glands but are much less abundant in their distribution than eccrine glands. They can be found in the axillary, ar—eolar, and anal regions.
Secretory portions of these glands are composed of a single layer of cuboidal or columnar cells. They are larger and have a much wider luminal diameter than eccrine sweat glands. Myoepithelial cells surround the secretory cells within the basement membrane and contract to facilitate secretion.
Duct portions are similar to those of eccrine sweat glands but open onto hair follicles instead of onto the epidermal surfaces.
Functions of these glands in humans is not at all clear. Specialized apocrine glands in the ear canal (ceruminous glands) produce a secretion in conjunction with adjacent sebaceous glands to form the protective earwax (cerumen). Control of the apocrine glands is hormonal and via the innervation of adrenergic fibers. These glands do not begin to function until puberty.
Sebaceous glands are simple, branched holocrine aci—nar glands. They usually discharge their secretions onto the hair shaft within hair follicles. These glands are found in the dermis throught the skin, except on the palms and soles.
Secretory portions consist of peripherally located, flattened stem cells that resemble basal keratinocytes. Toward the center of the acini, enlarged differentiated cells are engorged with lipid. Death and fragmentation of cells nearest the duct portion result in the holocrine mechanism of secretion.
Duct portions of sebaceous glands are composed of stratified squamous epithelium that is continuous with the hair cat and epidermal surface.
Functions involve the lubrication of both hairs and corni—fied layers of the skin, as well as resistance to desiccation.
Control of sebaceous glands is hormonal. Enlargement of the acini occurs at puberty.
Hairs are long, filamentous projections consisting of dead keratini—zed epidermal cells. Each hair derives from an epidermal invagination called the hair follicle, which possesses a terminal hair bulb, located in the dermis or hypo—dermis, from which the hair shaft grows. Contraction of smooth muscles raise the hairs and dimple the epidermis («goose flesh»).
Nails, like hair, are a modified stratum corneum of the epidermis. They contain hard keratin that forms in a manner similar to the formation of hair. Cells continually proliferate and keratinize from the stratum basale of the nail matrix.
New words
cutaneous – кожный
appendace – покров
tubular – трубчатый
pyramidal – пирамидальный
surface – поверхность
thermal – тепловой
innervation – иннервация
7. Matter
Matter is anything that occupies space, possesses mass and can be perceived by our sense organs. It exists in nature in three, usually inter convertible physical states: solids, liquids and gases. For instance, ice, water and steam are respectively the solid, liquid and gaseous states of water. Things in the physical world are made up of a relatively small number of basic materials combined in various ways. The physical material of which everything that we can see or touch is made is matter. Matter exists in three different states: solid, liquid and gaseous. Human senses with the help of tools allow us to determine the properties of matter. Matter can undergo a variety of changes – physical and chemical, natural and controlled.
Chemistry and physics deal with the study of matter, its properties, changes and transformation with energy. There are two kinds of properties: physical – colour, taste, odour, density, hardness, solubility and ability to conduct electricity and heat; in solids the shape of their crystals is significant, freezing and boiling points of liquids.
Chemical properties are the changes in composition undergone by a substance when it is subjected to various conditions. The various changes may be physical and chemical. The physical properties are temporary. In a chemical change the composition of the substance is changed and new products are formed. Chemical properties are permanent.
It is useful to classify materials as solid, liquid or gas (though water, for example, exists as solid (ice), as liquid (water) and as gas (water vapour). The changes of state described by the terms solidify (freeze), liquify (melt), va—pourise (evaporate) and condense are examples of physical changes. After physical change there is still the same material. Water is water whether it is solid, liquid or gas. Also, there is still the same mass of material. It is usually easy to reverse a physical change.
New words
matter – материя
mass – масса
sense – чувство
organ – орган
steam – пар
to undergo – подвергать
variety – разнообрзие
change – перемена
physical – физический
chemical – химический
natural – природный
transformation – трансформация
colour – цвет
taste – вкус
odour – запах
density – плотность
hardness – твердость
solubility – растворимость
ability – возможность
to conduct – проводить
permanent – постоянный
Chemistry and physics deal with the study of matter, its properties, changes and transformation with energy. There are two kinds of properties: physical – colour, taste, odour, density, hardness, solubility and ability to conduct electricity and heat; in solids the shape of their crystals is significant, freezing and boiling points of liquids.
Chemical properties are the changes in composition undergone by a substance when it is subjected to various conditions. The various changes may be physical and chemical. The physical properties are temporary. In a chemical change the composition of the substance is changed and new products are formed. Chemical properties are permanent.
It is useful to classify materials as solid, liquid or gas (though water, for example, exists as solid (ice), as liquid (water) and as gas (water vapour). The changes of state described by the terms solidify (freeze), liquify (melt), va—pourise (evaporate) and condense are examples of physical changes. After physical change there is still the same material. Water is water whether it is solid, liquid or gas. Also, there is still the same mass of material. It is usually easy to reverse a physical change.
New words
matter – материя
mass – масса
sense – чувство
organ – орган
steam – пар
to undergo – подвергать
variety – разнообрзие
change – перемена
physical – физический
chemical – химический
natural – природный
transformation – трансформация
colour – цвет
taste – вкус
odour – запах
density – плотность
hardness – твердость
solubility – растворимость
ability – возможность
to conduct – проводить
permanent – постоянный
8. Skeletal system
The components of the skeletal system are derived from mesenchymal elements that arise from mesoderm and neural crest. Mesenchymal cells differentiate into fibroblasts, chondroblasts, and osteoblasts, which produce connective tissue, cartilage, and bone tissue, respectively. Bone organs either develop directly in mesenchymal connective tissue (intramembranous ossification) or from preformed cartilage models (endochondral ossification). The splanch nic meso—derm gives rise to cardiac and smooth muscle.
The skeletal system develops from paraxial mesoderm. By the end of the fourth week, the sclerotome cells form embryonic connective tissue, known as mesenchyme. Mesenchyme cells migrate and differentiate to form fibro—blasts, chondroblasts, or osteoblasts.
Bone organs are formed by two methods.
Flat bones are formed by a process known as intra—membinous ossification, in which bones develop directly within mesenchyme.
Long bones are formed by a process known as en—dochondral ossification, in which mesenchymal cells give rise hyaline cartilage models that subsequently become ossified.
Skull formation.
Neurocranium is divided into two portions: The membranous neurocranium consists of flat bones that surround the brain as a vault. The bones appose one another at sutures and fontanelles, which allow overlap of bones during birth and remain membranous until adulthood.
The cartilaginous neurocranium (chondro—cranium) of the base of the skull is formed by fusion and ossification of number of separate cartilages along the median plate.
Viscerocranium arises primarily from the first two pharynge arches.
Appendicular system: The pectoral and pelvic girdles and the limbs comprise the appendicular system.
Except for the clavicle, most bones of the system are end chondral. The limbs begin as mesenchymal buds with an apical ectodermal ridge covering, which exerts an inductive influence over the mesenchyme.
Bone formation occurs by ossification of hyaline cartilage models.
The cartilage that remains between the diaphysis and the epiphyses of a long bone is known as the epiphysial plate. It is the site of growth of long bones until they attain their final size and the epiphysial plate disappears.
Vertebral column.
During the fourth week, sclerotome cells migrate medially to surround the spinal cord and notochord. After proliferation of the caudal portion of the sclerotomes, the vertebrae are formed, each consisting of the caudal part of one sclerotome and cephalic part of the next.
While the notochord persists in the areas of the vertebral bod ies, it degenerates between them, forming the nucleus pulposus. The latter, together with surrounding circular fibers of the annulus fibrosis, forms the intervertebral disc.
New words
skeletal – скелетный
mesoderm – мезодерма
cartilage – хрящ
fibroblasts – фибробласты
chondroblasts – хондробласты
osteoblasts – остеобласты
paraxial – параксиальный
flat – плоский
bone – кость
The skeletal system develops from paraxial mesoderm. By the end of the fourth week, the sclerotome cells form embryonic connective tissue, known as mesenchyme. Mesenchyme cells migrate and differentiate to form fibro—blasts, chondroblasts, or osteoblasts.
Bone organs are formed by two methods.
Flat bones are formed by a process known as intra—membinous ossification, in which bones develop directly within mesenchyme.
Long bones are formed by a process known as en—dochondral ossification, in which mesenchymal cells give rise hyaline cartilage models that subsequently become ossified.
Skull formation.
Neurocranium is divided into two portions: The membranous neurocranium consists of flat bones that surround the brain as a vault. The bones appose one another at sutures and fontanelles, which allow overlap of bones during birth and remain membranous until adulthood.
The cartilaginous neurocranium (chondro—cranium) of the base of the skull is formed by fusion and ossification of number of separate cartilages along the median plate.
Viscerocranium arises primarily from the first two pharynge arches.
Appendicular system: The pectoral and pelvic girdles and the limbs comprise the appendicular system.
Except for the clavicle, most bones of the system are end chondral. The limbs begin as mesenchymal buds with an apical ectodermal ridge covering, which exerts an inductive influence over the mesenchyme.
Bone formation occurs by ossification of hyaline cartilage models.
The cartilage that remains between the diaphysis and the epiphyses of a long bone is known as the epiphysial plate. It is the site of growth of long bones until they attain their final size and the epiphysial plate disappears.
Vertebral column.
During the fourth week, sclerotome cells migrate medially to surround the spinal cord and notochord. After proliferation of the caudal portion of the sclerotomes, the vertebrae are formed, each consisting of the caudal part of one sclerotome and cephalic part of the next.
While the notochord persists in the areas of the vertebral bod ies, it degenerates between them, forming the nucleus pulposus. The latter, together with surrounding circular fibers of the annulus fibrosis, forms the intervertebral disc.
New words
skeletal – скелетный
mesoderm – мезодерма
cartilage – хрящ
fibroblasts – фибробласты
chondroblasts – хондробласты
osteoblasts – остеобласты
paraxial – параксиальный
flat – плоский
bone – кость
9. Muskular system
Skeletal (voluntary) system.
The dermomyotome further differentiates into the myo—tome and the dermatome.
Cells of the myotome migrate ventrally to surround the in—traembryonic coelom and the somatic mesoderm of the ventrolateral body wall. These myoblasts elongate, become spindle—shaped, and fuse to form multinucleated muscle fibers.
Myofibrils appear in the cytoplasm, and, by the third month, cross—striations appear. Individual muscle fibers increase in diameter as myofibrils multiply and become arranged in groups surrounded by mesenchyme.
Individual muscles form, as well as tendons that connect muscle to bone.
Trunk musculature: By the end of the fifth week, body—wall musculature divides into a dorsal epimere, supplied by the dorsal primary ramus of the spinal nerve, and a ventral hypomere, supplied by the ventral primary ramus.
Epimere muscles form the extensor muscles of the vertebral column, and hypomere muscles give rise to lateral and ven tral flexor musculature.
The hypomere splits into three layers. In the thorax, the three layers form the external costal, internal intercostal, and transverse thoracic muscle.
In the abdomen, the three layers form the external oblique, internal oblique, and transverse abdomii muscles.
Head musculature.
The extrinsic and intrinsic muscles of the tongue are thought to be derived from occipital myotomes that migrate forward.
The extrinsic muscles of the eye may derive from preop—tic myotomes that originally surround the prochordal plate.
The muscles of mastication, facial expression, the pharynx, and the larynx are derived from different pharyngeal arches and maintain their innervation by the nerve of the arch of origin.
Limb musculature originates in the seventh week from soma mesoderm that migrates into the limb bud. With time, the limb musculature splits into ventral flexor and dorsal extern groups.
The limb is innervated by spinal nerves, which penetrate the limb bud mesodermal condensations. Segmental branches of the spinal nerves fuse to form large dorsal a ventral nerves.
The cutaneous innervation of the limbs is also derived from spinal nerves and reflects the level at which the limbs arise.
Smooth muscle: the smooth muscle coats of the gut, trachtea, bronchi, and blood vessels of the associated mesenteries are derived from splanchnic mesoderm surrounding the gastrointestinal tract. Vessels elsewhere in the body obtain their coat from local mesenchyme.
Cardiac muscle, like smooth muscle, is derived from splanchnic mesoderm.
New words
ventral – брюшной
somatic – соматический
cytoplasm – цитоплазма
cross—striations – поперечные бороздчатости
extensor – разгибающая мышца
dorsal – спинной
ivertebral – позвоночный
arche – дуга
abdomen – живот
facial – лицевой
branch – ветвь
The dermomyotome further differentiates into the myo—tome and the dermatome.
Cells of the myotome migrate ventrally to surround the in—traembryonic coelom and the somatic mesoderm of the ventrolateral body wall. These myoblasts elongate, become spindle—shaped, and fuse to form multinucleated muscle fibers.
Myofibrils appear in the cytoplasm, and, by the third month, cross—striations appear. Individual muscle fibers increase in diameter as myofibrils multiply and become arranged in groups surrounded by mesenchyme.
Individual muscles form, as well as tendons that connect muscle to bone.
Trunk musculature: By the end of the fifth week, body—wall musculature divides into a dorsal epimere, supplied by the dorsal primary ramus of the spinal nerve, and a ventral hypomere, supplied by the ventral primary ramus.
Epimere muscles form the extensor muscles of the vertebral column, and hypomere muscles give rise to lateral and ven tral flexor musculature.
The hypomere splits into three layers. In the thorax, the three layers form the external costal, internal intercostal, and transverse thoracic muscle.
In the abdomen, the three layers form the external oblique, internal oblique, and transverse abdomii muscles.
Head musculature.
The extrinsic and intrinsic muscles of the tongue are thought to be derived from occipital myotomes that migrate forward.
The extrinsic muscles of the eye may derive from preop—tic myotomes that originally surround the prochordal plate.
The muscles of mastication, facial expression, the pharynx, and the larynx are derived from different pharyngeal arches and maintain their innervation by the nerve of the arch of origin.
Limb musculature originates in the seventh week from soma mesoderm that migrates into the limb bud. With time, the limb musculature splits into ventral flexor and dorsal extern groups.
The limb is innervated by spinal nerves, which penetrate the limb bud mesodermal condensations. Segmental branches of the spinal nerves fuse to form large dorsal a ventral nerves.
The cutaneous innervation of the limbs is also derived from spinal nerves and reflects the level at which the limbs arise.
Smooth muscle: the smooth muscle coats of the gut, trachtea, bronchi, and blood vessels of the associated mesenteries are derived from splanchnic mesoderm surrounding the gastrointestinal tract. Vessels elsewhere in the body obtain their coat from local mesenchyme.
Cardiac muscle, like smooth muscle, is derived from splanchnic mesoderm.
New words
ventral – брюшной
somatic – соматический
cytoplasm – цитоплазма
cross—striations – поперечные бороздчатости
extensor – разгибающая мышца
dorsal – спинной
ivertebral – позвоночный
arche – дуга
abdomen – живот
facial – лицевой
branch – ветвь
10. Skeleton
The bones of our body make up a skeleton. The skeleton forms about 18 % of the weight of the human body.
The skeleton of the trunk mainly consists of spinal column made of a number of bony segments called vertebrae to which the head, the thoracic cavity and the pelvic bones are connected. The spinal column consists of 26 spinal column bones.
The human vertebrae are divided into differentiated groups. The seven most superior of them are the vertebrae called the cervical vertebrae. The first cervical vertebra is the atlas. The second vertebra is called the axis.
Inferior to the cervical vertebrae are twelve thoracic vertebrae. There is one rib connected to each thoracic vertebrae, making 12 pairs of ribs. Most of the rib pairs come together ventrally and join a flat bone called the sternum.
The first pairs or ribs are short. All seven pairs join the sternum directly and are sometimes called the «true ribs». Pairs 8, 9, 10 are «false ribs». The eleventh and twelfth pairs of ribs are the «floating ribs».
Inferior to the thoracic vertebrae are five lumbar vertebrae. The lumbar vertebrae are the largest and the heaviest of the spinal column. Inferior to the lumbar vertebrae are five sacral vertebrae forming a strong bone in adults. The most inferior group of vertebrae are four small vertebrae forming together the соссуж.
The vertebral column is not made up of bone alone. It also has cartilages.
New words
skeleton – скелет
make up – составлять
weight – вес
trunk – туловище
vertebrae – позвоночник
thoracic cavity – грудная клетка
pelvic – тазовый
cervical – шейный
atlas – 1 шейный позвонок
sternum – грудина
mainly – главным образом
axis – ось
spinal column – позвоночник
inferior – нижний
rib – ребро
pair – пара
sacral – сакральный
соссу«– копчик
floating – плавающий
forming – формирующий
cartilage – хрящ
lumbar – поясничный
adult – взрослый
The skeleton of the trunk mainly consists of spinal column made of a number of bony segments called vertebrae to which the head, the thoracic cavity and the pelvic bones are connected. The spinal column consists of 26 spinal column bones.
The human vertebrae are divided into differentiated groups. The seven most superior of them are the vertebrae called the cervical vertebrae. The first cervical vertebra is the atlas. The second vertebra is called the axis.
Inferior to the cervical vertebrae are twelve thoracic vertebrae. There is one rib connected to each thoracic vertebrae, making 12 pairs of ribs. Most of the rib pairs come together ventrally and join a flat bone called the sternum.
The first pairs or ribs are short. All seven pairs join the sternum directly and are sometimes called the «true ribs». Pairs 8, 9, 10 are «false ribs». The eleventh and twelfth pairs of ribs are the «floating ribs».
Inferior to the thoracic vertebrae are five lumbar vertebrae. The lumbar vertebrae are the largest and the heaviest of the spinal column. Inferior to the lumbar vertebrae are five sacral vertebrae forming a strong bone in adults. The most inferior group of vertebrae are four small vertebrae forming together the соссуж.
The vertebral column is not made up of bone alone. It also has cartilages.
New words
skeleton – скелет
make up – составлять
weight – вес
trunk – туловище
vertebrae – позвоночник
thoracic cavity – грудная клетка
pelvic – тазовый
cervical – шейный
atlas – 1 шейный позвонок
sternum – грудина
mainly – главным образом
axis – ось
spinal column – позвоночник
inferior – нижний
rib – ребро
pair – пара
sacral – сакральный
соссу«– копчик
floating – плавающий
forming – формирующий
cartilage – хрящ
lumbar – поясничный
adult – взрослый
11. Muscles
Muscles are the active part of the motor apparatus; their contraction produces various movements.
The muscles may be divided from a physiological standpoint into two classes: the voluntary muscles, which are under the control of the will, and the involuntary muscles, which are not.
All muscular tissues are controlled by the nervous system.
When muscular tissue is examined under the microscope, it is seen to be made up of small, elongated threadlike cells, which arc called muscle fibres, and which are bound into bundles by connective tissue.
There are three varieties of muscle fibres:
1) striated muscle fibres, which occur in voluntary muscles;
2) unstriated muscles which bring about movements in the internal organs;
3) cardiac or heart fibres, which are striated like (1), but are otherwise different.
Muscle consists of threads, or muscle fibers, supported by connective tissue, which act by fiber contraction. There are two types of muscles smooth and striated. Smooth, muscles are found in the walls of all the hollow organs and tubes of the body, such as blood vessels and intestines. These react slowly to stimuli from the autonomic nervous system. The striated, muscles of the body mostly attach to the bones and move the skeleton. Under the microscope their fibres have a cross – striped appearance. Striated muscle is capable of fast contractions. The heart wall is made up of special type of striated muscle fibres called cardiac muscle. The body is composed of about 600 skeletal muscles. In the adult about 35–40 % of the body weight is formed by the muscles. According to the basic part of the skeleton all the muscles are divided into the muscles of the trunk, head and extremities.
According to the form all the muscles are traditionally divided into three basic groups: long, short and wide muscles. Long muscles compose the free parts of the extremities. The wide muscles form the walls of the body cavities. Some short muscles, of which stapedus is the smallest muscle in the human body, form facial musculature.
Some muscles are called according to the structure of their fibres, for example radiated muscles; others according to their uses, for example extensors or according to their directions, for example, – oblique.
Great research work was carried out by many scientists to determine the functions of the muscles. Their work helped to establish that the muscles were the active agents of motion and contraction.
New words
muscles – мышцы active – активный
motor apparatus – двигательный аппарат
various – различный
movement – движение
elongated – удлиненный
threadlike – нитевидный
be bound – быть связанным
ability – возможность
capable – способность
scientist – ученый
basic – основной
The muscles may be divided from a physiological standpoint into two classes: the voluntary muscles, which are under the control of the will, and the involuntary muscles, which are not.
All muscular tissues are controlled by the nervous system.
When muscular tissue is examined under the microscope, it is seen to be made up of small, elongated threadlike cells, which arc called muscle fibres, and which are bound into bundles by connective tissue.
There are three varieties of muscle fibres:
1) striated muscle fibres, which occur in voluntary muscles;
2) unstriated muscles which bring about movements in the internal organs;
3) cardiac or heart fibres, which are striated like (1), but are otherwise different.
Muscle consists of threads, or muscle fibers, supported by connective tissue, which act by fiber contraction. There are two types of muscles smooth and striated. Smooth, muscles are found in the walls of all the hollow organs and tubes of the body, such as blood vessels and intestines. These react slowly to stimuli from the autonomic nervous system. The striated, muscles of the body mostly attach to the bones and move the skeleton. Under the microscope their fibres have a cross – striped appearance. Striated muscle is capable of fast contractions. The heart wall is made up of special type of striated muscle fibres called cardiac muscle. The body is composed of about 600 skeletal muscles. In the adult about 35–40 % of the body weight is formed by the muscles. According to the basic part of the skeleton all the muscles are divided into the muscles of the trunk, head and extremities.
According to the form all the muscles are traditionally divided into three basic groups: long, short and wide muscles. Long muscles compose the free parts of the extremities. The wide muscles form the walls of the body cavities. Some short muscles, of which stapedus is the smallest muscle in the human body, form facial musculature.
Some muscles are called according to the structure of their fibres, for example radiated muscles; others according to their uses, for example extensors or according to their directions, for example, – oblique.
Great research work was carried out by many scientists to determine the functions of the muscles. Their work helped to establish that the muscles were the active agents of motion and contraction.
New words
muscles – мышцы active – активный
motor apparatus – двигательный аппарат
various – различный
movement – движение
elongated – удлиненный
threadlike – нитевидный
be bound – быть связанным
ability – возможность
capable – способность
scientist – ученый
basic – основной
12. Bones
Bone is the type of connective tissue that forms the body's supporting framework, the skeleton. Serve to protect the internal organs from injury. The bone marrow inside the bones is the body's major producer of both red and white blood cells.
The bones of women are generally lighter than those of men, while children's bones are more resilient than those of adults. Bones also respond to certain physical physiological changes: atrophy, or waste away.
Bones are generally classified in two ways. When classified on the basis of their shape, they fall into four categories: flat bones, such as the ribs; long bones, such as the thigh bone; short bones, such as the wrist bones; and irregular bones, such as the vertebrae. When classified on the basis of how they develop, bones are divided into two groups: en—dochondral bones and intramembraneous bones. En—dochondral bones, such as the long bones and the bones at the base of the skull, develop from cartilage tissue. Intra—membraneous bones, such as the flat bones of the roof of the skull, are not formed from cartilage but develop under or within a connective tissue membrane. Although en—dochondral bones and intramembraneous bones form in different ways, they have the same structure.
The formation of bone tissue (ossification) begins early in embryological development. The bones reach their full size when the person is about 25.
Most adult bone is composed of two types of tissue: anouter layer of compact bone and an inner layer of spongy bone. Compact bone is strong and dense. Spongy bone is light and porous and contains bone marrow. The amount of each type of tissue varies in different bones. The flat bones of the skull consist almost entirely of com pact bone, with very little spongy tissue. In a long bone, such as the thigh bone, the shaft, called the diaphysis, is made up largely of compact bone. While the ends, called epyphyses, consist mostly of spongy bone. In a long bone, marrow is also present inside the shaft, in a cavity called the medullary cavity.
Surrounding every bone, except at the surface where it meets another bone, is a fibrous membrane called the periosteum. The outer layer of the periosteum consists of a network of densely packed collagen fibres and blood vessels. This layer serves for the attachment of tendons, ligaments, and muscles to the bone and is also important in bone repair.
The inner layer of the periosteum has many fibres, called fibres of Sharpey, which penetrate the bone tissue, anchoring the periosteum to the bone. The inner layer also has many bone—forming cells, or osteoblasts, which are responsible for the bone's growth in diameter and the production of new bone tissue in cases of fracture, infection.
In addition to the periosteum, all bones have another membrane, the endosteum. It lines the marrow cavity as well as the smaller cavities within the bone. This membrane, like the inner layer of the periosteum, contains os—teoblasts, and is important in the formation of new bone tissue.
The bones of women are generally lighter than those of men, while children's bones are more resilient than those of adults. Bones also respond to certain physical physiological changes: atrophy, or waste away.
Bones are generally classified in two ways. When classified on the basis of their shape, they fall into four categories: flat bones, such as the ribs; long bones, such as the thigh bone; short bones, such as the wrist bones; and irregular bones, such as the vertebrae. When classified on the basis of how they develop, bones are divided into two groups: en—dochondral bones and intramembraneous bones. En—dochondral bones, such as the long bones and the bones at the base of the skull, develop from cartilage tissue. Intra—membraneous bones, such as the flat bones of the roof of the skull, are not formed from cartilage but develop under or within a connective tissue membrane. Although en—dochondral bones and intramembraneous bones form in different ways, they have the same structure.
The formation of bone tissue (ossification) begins early in embryological development. The bones reach their full size when the person is about 25.
Most adult bone is composed of two types of tissue: anouter layer of compact bone and an inner layer of spongy bone. Compact bone is strong and dense. Spongy bone is light and porous and contains bone marrow. The amount of each type of tissue varies in different bones. The flat bones of the skull consist almost entirely of com pact bone, with very little spongy tissue. In a long bone, such as the thigh bone, the shaft, called the diaphysis, is made up largely of compact bone. While the ends, called epyphyses, consist mostly of spongy bone. In a long bone, marrow is also present inside the shaft, in a cavity called the medullary cavity.
Surrounding every bone, except at the surface where it meets another bone, is a fibrous membrane called the periosteum. The outer layer of the periosteum consists of a network of densely packed collagen fibres and blood vessels. This layer serves for the attachment of tendons, ligaments, and muscles to the bone and is also important in bone repair.
The inner layer of the periosteum has many fibres, called fibres of Sharpey, which penetrate the bone tissue, anchoring the periosteum to the bone. The inner layer also has many bone—forming cells, or osteoblasts, which are responsible for the bone's growth in diameter and the production of new bone tissue in cases of fracture, infection.
In addition to the periosteum, all bones have another membrane, the endosteum. It lines the marrow cavity as well as the smaller cavities within the bone. This membrane, like the inner layer of the periosteum, contains os—teoblasts, and is important in the formation of new bone tissue.
13. Bones. Chemical structure
Bone tissue consists largely of a hard substance called the matrix. Embedded in the matrix are the bone cells, or osteocytes. Bone matrix consists of both organic and inorganic materials. The organic portion is made up chiefly of collagen fibres. The inorganic portion of matrix constitutes about two thirds of a bone's total weight. The chief inorganic substance is calcium phosphate, which is responsible for the bone's hardness. If the organic portion were burned out the bone would crumble under the slightest pressure. In the formation of intramembraneous bone, certain cells of the embryonic connective tissue congregate in the area where the bone is to form. Small blood vessels soon invade the area, and the cells, which have clustered in strands, undergo certain changes to become osteoblasts. The cells then begin secreting collagen fibers and an intercellular substance. This substance, together with the collagen fibers and the connective tissue fibers already present, is called osteoid. Osteoid is very soft and flexible, but as mineral salts are deposited it becomes hard matrix. The formation of endochondral bone is preceded by the formation of a cartilaginous structure similar in shape to the resulting bone. In a long bone, ossification begins in the area that becomes the center of the shaft. In this area, cartilage cells become osteoblasts and start forming bone tissue. This process spreads toward either end of the bone. The only areas where cartilage is not soon replaced by bone tissue are the regions where the shaft joins the two epiphyses. These areas, called epiphyseal pla—res, are responsible for the bone's continuing growth in length. The bone's growth in diameter is due to the addition of layers of bone around the outside of the shaft. As they are formed, layers of bone on the inside of the shaft are removed. In all bones, the matrix is arranged in layers called lamellae. In compact bone, the lamellae are arranged concentrically around blood vessels, and the space containing each blood vessel is called a Haver—sian canal. The osteocytes are located between the lamellae, and the canaliculi containing their cellular extensions connect with the Haversian canals, allowing the passage of nutrients and other materials between the cells and the blood vessels. Bone tissue contains also many smaller blood vessels that extend from the periosteum and enter the bone through small openings. In long bones there is an additional blood supply, the nutrient artery, which represents the chief blood supply to the marrow. The structure of spongy is similar to that of compact bone. However, there are fewer Haversian canals, and the lamellae are arranged in a less regular fashion, forming spicules and strands known as trabeculae.
New words
bone – кость
internal – внешний
phosphorus – фосфор
atrophy – атрофия
spongy – губчатый
tendon – сухожилие
ligament – связка
flexible – гибкий
periosteum – надкостница
osteoblast – остеобласт (клетка, образующая кость)
rigidity – неподвижность
shape – форма
to crumble – крошиться
to congregate – собираться
epiphyseal – относящийся к эпифизу
shaft – ствол, тело (длинной) кости, диафиз
New words
bone – кость
internal – внешний
phosphorus – фосфор
atrophy – атрофия
spongy – губчатый
tendon – сухожилие
ligament – связка
flexible – гибкий
periosteum – надкостница
osteoblast – остеобласт (клетка, образующая кость)
rigidity – неподвижность
shape – форма
to crumble – крошиться
to congregate – собираться
epiphyseal – относящийся к эпифизу
shaft – ствол, тело (длинной) кости, диафиз
14. Skull
Bones of the skull: the neurocranium (the portion of the skull that surrounds and protects the brain) or the viscerocra—nium (i. e., the skeleton of the face). Bones of the neurocrani—um: Frontal, Parietal, Temporal, Occipital, Ethmoid, Sphenoid.
Bones of the viscerocranium (surface): Maxilla, Nasal, Zy—gomatic, Mandible. Bones of the viscerocranium (deep): Ethmoid, Sphenoid, Vomer, Lacrimal, Palatine, Inferior nasal concha. Articulations: Most skull bones meet at immovable joints called sutures. The coronal suture is between the frontal and the parietal bones. The sagittal suture is between two parietal bones. The lambdoid suture is between the parietal and the occipital bones. The bregma is the point at which the coronal suture intersects the sagittal suture.
The lambda is the point at which the sagittal suture intersects the lambdoid suture. The pterion is the point on the lateral aspect of the skull where the greater wing of the sphenoid, parietal, frontal, and temporal bones converge. The temporomandibular joint is between the mandibular fossa of the temporal bone and the condylar process of the mandible.
The parotid gland is the largest of the salivary glands. Structures found within the substance of this gland include the following: Motor branches of the facial nerve. CN VII enters the parotid gland after emerging from the stylomastoid foramen at the base of the skull. Superficial temporal artery and vein. The artery is a terminal branch of the external carotid artery.
Retromandibular vein, which is formed from the maxillary and superficial temporal veins.
Great auricular nerve, which is a cutaneous branch of the cer vical plexus. Auriculotemporal nerve, which is a sensory branch of V3. It supplies the TMJ and conveys postganglionic parasympathetic fibers from the otic ganglion to the parotid gland. Parotid (Stensen's) duct, which enters the oral cavity at the level of the maxillary second molar. The facial artery is a branch of the external carotid artery in the neck. It terminates as the angular artery near the bridge of the nose.
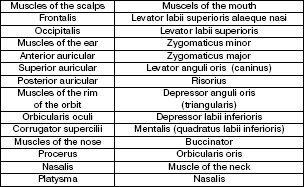
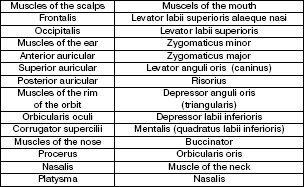
The muscles of face
New words
brain – мозг
frontal – лобная
parietal – теменная
temporal – височная
occipital – затылочная
ethmoid – решетчатая
maxilla – верхняя челюсть
zygomatic – скуловой
mandible – нижняя челюсть
sphenoid – клиновидная
vomer – сошник
lacrimal – слезная
palatine – небная
nasal concha – носовая раковина
Bones of the viscerocranium (surface): Maxilla, Nasal, Zy—gomatic, Mandible. Bones of the viscerocranium (deep): Ethmoid, Sphenoid, Vomer, Lacrimal, Palatine, Inferior nasal concha. Articulations: Most skull bones meet at immovable joints called sutures. The coronal suture is between the frontal and the parietal bones. The sagittal suture is between two parietal bones. The lambdoid suture is between the parietal and the occipital bones. The bregma is the point at which the coronal suture intersects the sagittal suture.
The lambda is the point at which the sagittal suture intersects the lambdoid suture. The pterion is the point on the lateral aspect of the skull where the greater wing of the sphenoid, parietal, frontal, and temporal bones converge. The temporomandibular joint is between the mandibular fossa of the temporal bone and the condylar process of the mandible.
The parotid gland is the largest of the salivary glands. Structures found within the substance of this gland include the following: Motor branches of the facial nerve. CN VII enters the parotid gland after emerging from the stylomastoid foramen at the base of the skull. Superficial temporal artery and vein. The artery is a terminal branch of the external carotid artery.
Retromandibular vein, which is formed from the maxillary and superficial temporal veins.
Great auricular nerve, which is a cutaneous branch of the cer vical plexus. Auriculotemporal nerve, which is a sensory branch of V3. It supplies the TMJ and conveys postganglionic parasympathetic fibers from the otic ganglion to the parotid gland. Parotid (Stensen's) duct, which enters the oral cavity at the level of the maxillary second molar. The facial artery is a branch of the external carotid artery in the neck. It terminates as the angular artery near the bridge of the nose.
The muscles of face
New words
brain – мозг
frontal – лобная
parietal – теменная
temporal – височная
occipital – затылочная
ethmoid – решетчатая
maxilla – верхняя челюсть
zygomatic – скуловой
mandible – нижняя челюсть
sphenoid – клиновидная
vomer – сошник
lacrimal – слезная
palatine – небная
nasal concha – носовая раковина
15. Neck. Cervical vertebrae, cartilages, triangels
Cervical vertebrae: There are seven cervical vertebrae of which the first two are atypical. All cervical vertebrae have the foramina transversaria which produce a canal that transmits the vertbral artery and vein.
Atlas: This is the first cervical vertebra (C1). It has no body and leaves a space to accommodate the dens of the second cervical vertebra. Axis: This is the second cervical vertebra (C2). It has odontoid process, which articulates with the atlas as a pivot joint. Hyoid bone is a small U—shaped bone, which is suspended by muscles and ligaments at the level of vertebra C3.
Laryngeal prominence is formed by the lamina of the thyroid cartilage.
Cricoid cartilage. The arch of the cricoid is palpable below the thyroid cartilage and superior to the first tracheal ring (vertebral level C6). Triangles of the neck: The neck is divided into a posterior and an arterior triangle by the sternocleidomastoid muscle. These triangles are subdivided by smaller muscles into six smaller triangles. Posterior triangle is bound by the sternocleidomastoid, the clavicle, and the trapezius. Occipital triangle is located above the inferior belly of the omohyoid muscle. Its contents include the following: CN XI Cutaneous branches of the cervical plexus are the lesser occipital, great auricular, transverse cervical, and supaclavicular nerves.
Subclavian (omoclavicular, supraclavicular) triangle is located below the inferior belly of the omohyoid. Its contents include the following: Brachial plexus supraclavicu—lar portion The branches include the dorsal scapular, long thoracic, subclavius, and suprascapular nerves.
The third part of the subclavian artery enters the subclavian triangle.
The subclavian vein passes superficial to scalenus anterior muscle. It receives the external jugular vein.
Atlas: This is the first cervical vertebra (C1). It has no body and leaves a space to accommodate the dens of the second cervical vertebra. Axis: This is the second cervical vertebra (C2). It has odontoid process, which articulates with the atlas as a pivot joint. Hyoid bone is a small U—shaped bone, which is suspended by muscles and ligaments at the level of vertebra C3.
Laryngeal prominence is formed by the lamina of the thyroid cartilage.
Cricoid cartilage. The arch of the cricoid is palpable below the thyroid cartilage and superior to the first tracheal ring (vertebral level C6). Triangles of the neck: The neck is divided into a posterior and an arterior triangle by the sternocleidomastoid muscle. These triangles are subdivided by smaller muscles into six smaller triangles. Posterior triangle is bound by the sternocleidomastoid, the clavicle, and the trapezius. Occipital triangle is located above the inferior belly of the omohyoid muscle. Its contents include the following: CN XI Cutaneous branches of the cervical plexus are the lesser occipital, great auricular, transverse cervical, and supaclavicular nerves.
Subclavian (omoclavicular, supraclavicular) triangle is located below the inferior belly of the omohyoid. Its contents include the following: Brachial plexus supraclavicu—lar portion The branches include the dorsal scapular, long thoracic, subclavius, and suprascapular nerves.
The third part of the subclavian artery enters the subclavian triangle.
The subclavian vein passes superficial to scalenus anterior muscle. It receives the external jugular vein.
Конец бесплатного ознакомительного фрагмента
